On Monday evening Jen was given
a combination of medications, when combined caused her to completely crash. Jen was completely out of it, unable to remain
conscious, eyes in different directions. I spent 20 minutes keeping her awake, talking
about how we met, our life together, our kids.
The Drs conferred, Jen needed to
get to the ICU, FAST. As they were
wheeling her out of the room, they asked me if they had the directive to
intubate her if necessary. Wanting her
to be alive for her father and her kids, I said yes.
And then I made that dreaded call that no one wants to make. To her father to come down, and to my parents
to bring the kids, NOW. I thought time
had run out, and prayed that they could get here in time on New Year’s eve.
When they got her to the ICU they did not intubate her. They analyzed the various number s and symptoms
and decided that it was the combination of medications that had overly sedated
her and dropped her respiratory rate so low despite the low oxygen level. They administered an opiate blocker that
instantly revived her from overdosed to fully awake and fully aware of
everything going on. I’ve never seen
anything like it, and I never want to see it again.
But based on her condition, we still believed that time was
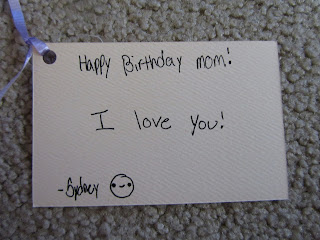
short. I had to tell the kids that Mom
might not have much time left. The
single most difficult thing I’ve ever had to do.
The girls and the parents were shuffled in and spent time
with her. By the end of the night, Jen
was doing better (a relative term), and it was determined that she would not
pass immediately. Exhausted, everybody
headed to our place in Franklin.
I walked everyone back to their cars with the assurance that
I would contact them if anything changed good or bad, and that everyone should
come back in the morning to see Jen
again.
I ran back up to the ICU just in time to give her a kiss at
new years. A moment I’ll never forget.
On Tuesday we meet with Dr.Santana and he gave us the bad
news. During the 2 week timeframe that
Jen had been off the crizotinib during the brain radiation treatment, the tumors
have progressed. It was determined that
Jen should receive a treatment of standard chemotherapy (in addition to the crizotinib)
to try to knock back the tumors. If the chemo can affect the cancer, there's a chance to get her in another clinical trial.
Jen spent the next three days in the ICU. Her plural effusions have been drained numerous times. And during that time,
she recovered from the imminent danger. She
was transferred back to the general lung patient floor on Thursday. Her lung function is returning slowly. Very slowly. But just as importantly, she’s getting a LOT
of sleep. She was incredibly sleep
deprived in the ICU, being poked, examined, and medicated every hour for 3 days.
So here we are again, in another hospital room. But it’s all the same. I’ve got nothing but prayer to effect the
situation. The ups, the downs, the endless
hours of waiting and hoping here are tough.
The next few days will determine if Jen gets to come
home. If her lung function comes up and
her oxygen requirements go down, maybe, just maybe, she can come home. The alternative is uncomfortable to
ponder. Today, we had a very serious
discussion of how hard she’s got to fight this and how I’m here with every step. She’s far from giving up. We’re far from giving up.